Introduction:
The advent of 3D printing technology has paved the way for groundbreaking advancements in various medical fields, including neurosurgical practice. The utilization of 3D printed neurovascular models has proven to be highly beneficial, offering significant advantages in surgical planning, training, and patient education. This article delves into the benefits of incorporating 3D printed neurovascular models in neurosurgical practice.
Precise Surgical Planning:
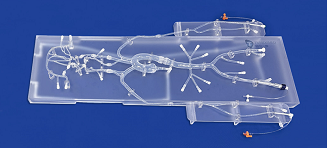
The 3D printed neurovascular model provides an accurate and detailed representation of complex neurovascular structures. Neurosurgeons can utilize these models to thoroughly analyze a patient's unique anatomy, identify critical structures, and plan intricate surgical procedures with precision. This enables surgeons to develop comprehensive surgical strategies, anticipate potential challenges, and enhance surgical outcomes by minimizing risks and optimizing patient safety.
Enhanced Training and Skills Development:
Training in neurosurgery requires mastering intricate techniques and understanding the intricacies of the neurovascular system. The 3D printed neurovascular model serves as an invaluable training tool, allowing neurosurgical residents and trainees to gain hands-on experience in a realistic and controlled environment. By practicing on the model, trainees can refine their skills, improve dexterity, and enhance their understanding of complex neurovascular interventions, ultimately leading to greater surgical proficiency.
Improved Patient Education and Informed Consent:
Neurosurgical procedures can be daunting and difficult for patients to comprehend, especially when it involves intricate neurovascular structures. The 3D printed neurovascular model bridges this gap by providing a tangible and visual representation of a patient's specific condition. Surgeons can use the model to explain the surgical approach, potential risks, and expected outcomes to patients and their families, facilitating better understanding and informed decision-making. This empowers patients to actively participate in their treatment journey, leading to improved patient satisfaction and compliance.
Personalized Treatment Approach:
Each patient's neurovascular anatomy is unique, and a one-size-fits-all approach may not always be optimal. With 3D printing technology, neurosurgeons can create patient-specific neurovascular models by incorporating imaging data, enabling personalized treatment planning. This customization facilitates preoperative simulations, allowing surgeons to evaluate different surgical strategies and select the most appropriate approach for each patient, resulting in improved surgical precision and patient outcomes.
Advancements in Research and Development:
3D printed neurovascular models have become invaluable tools for research and development in the field of neurosurgery. Researchers can utilize these models to study the efficacy of novel surgical techniques, test innovative devices, and explore new treatment modalities. The ability to replicate intricate neurovascular structures accurately provides a controlled environment for experimentation and fosters advancements in neurosurgical procedures and device design.
Conclusion:
The integration of 3D printed neurovascular models in neurosurgical practice offers immense benefits, ranging from precise surgical planning and enhanced training to improved patient education and personalized treatment approaches. These models empower neurosurgeons with a deeper understanding of complex neurovascular anatomy, leading to improved surgical outcomes and patient care. As 3D printing technology continues to evolve, the potential for neurovascular models in neurosurgical practice will expand, enabling further advancements in the field and ultimately benefiting patients worldwide.
Related product:
https://www.trando-med.com/medical-simulation/neuro-vessel-model/neuro-vascular.html