Common bile duct stones refer to stones located in the common bile duct and are a common and frequently-occurring disease in the biliary system. According to clinical surveys, the incidence rate in our country is about 4%-11%.
causes of common bile duct stones are hereditary abnormal cholesterol metabolism, cholestasis and infection of the biliary system. Bad living habits can increase the incidence, such as people who often eat hot pot, barbecue, egg yolks, animal offal and other greasy foods; people who often skip breakfast, go hungry every meal, and have irregular diets.
The clinical manifestations and harm of common bile duct stones. The most typical clinical manifestations of common bile duct stones are epigastric cramps and penetrating back pain, chills, high fever, and subsequent jaundice. If the lower end of the common bile duct is completely obstructed and the gallbladder If the tube is unobstructed, it may be manifested as a swollen and tender cystic mass in the right upper quadrant; the liver may also appear symmetrical, diffuse enlargement, and tenderness; the patient may present with high fever , which may lead to liver cell damage and biliary stasis, etc. Toxic symptoms, if you do not seek medical treatment in time or seek medical treatment late, the infection will be further aggravated, and symptoms of systemic toxemia and toxic shock will appear, which can be life-threatening in severe cases.
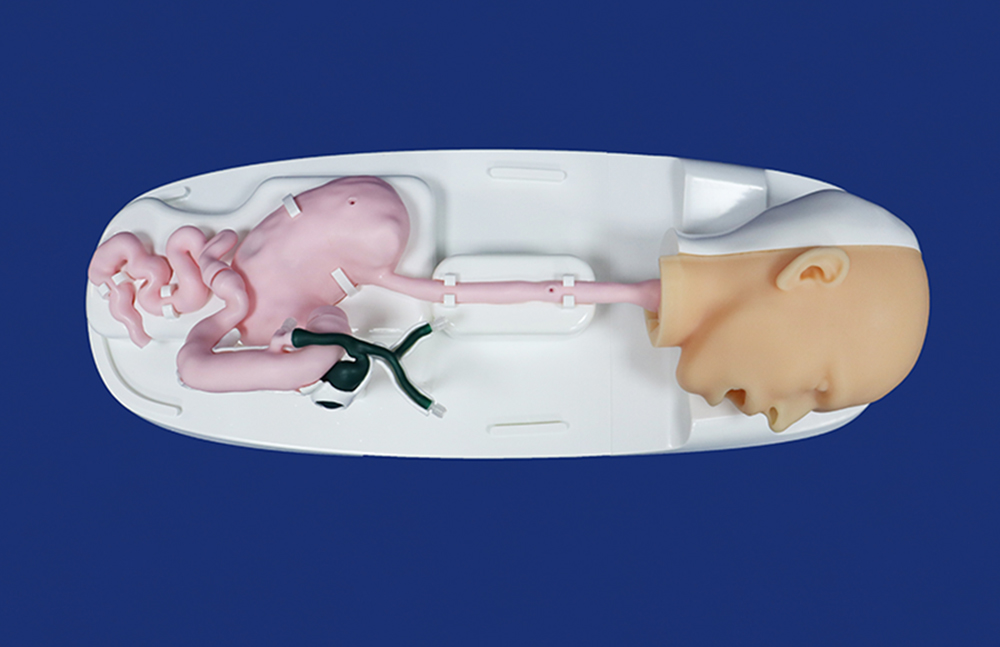
Why choose ERCP for treatment of common bile duct stones? ERCP is an imaging technique that injects contrast agent through the duodenal papilla under endoscopy to display the cholangiopancreatic duct retrogradely. It can be used for both the diagnosis and treatment of bile duct stones. With the continuous development of endoscopic equipment and technology, the use of ERCP lithotomy combined with laparoscopic cholecystectomy to treat common bile duct stones has gained wide recognition. To some extent, it has replaced laparotomy and become the current preferred treatment for extrahepatic bile duct stones. Laparotomy is a classic and standardized method for the clinical treatment of common bile duct stones. However, the operation is highly invasive and the postoperative recovery is slow. With the widespread use of ERCP in clinical practice, it has gained the favor of patients and doctors. This operation has the following advantages: It has the advantages of small trauma, short course of disease, good curative effect and few complications. Regardless of symptoms of common bile duct stones, ERCP is required to avoid manifestations of cholangitis such as fever, abdominal pain, jaundice, etc. Without surgery, some patients may induce biliary pancreatitis. Bile duct stones are easy to recur. If stones occur again, ERCP can be used to remove the stones, but laparotomy is relatively difficult to perform again.
Preparation for ERCP surgery . All bile duct stones should have B-ultrasound, CT imaging, and MRCP evidence. Routine examinations also need to be completed, including blood routine, blood biochemistry, coagulation function, chest X-ray, and electrocardiogram. Some elderly patients and those with underlying diseases The patient continued to undergo cardiac color ultrasound and pulmonary function tests. After preoperative discussion by the ERCP team, regarding the indications for surgery before surgery, the patient and the patient's family will be communicated to inform them of the indications, purpose of surgery, alternatives, and possible risks and complications. If the patient and the patient's family agree to the operation, fasting is required eight hours before the operation . Preoperative medication: a tube of dyclonine hydrochloride for local anesthesia of the throat, preparation of pethidine, atropine, and diazepam, intramuscular medication, and establishment of intravenous access. During the operation, oxygen inhalation and ECG monitoring were provided.
During the operation, surgical methods such as incision, balloon dilatation, and lithotripsy are selected according to the patient's specific conditions.
For postoperative observation, all surgical patients are routinely fasted for 24 hours after surgery and monitored by ECG. Blood routine and pancreatic enzyme spectrum will be reviewed on the second day after surgery. If no complications occur, they can eat after 24 hours.